Some years back, my mother was diagnosed with not one, but two chronic conditions. That was a difficult month for our family. I watched her and my father, who also suffers from chronic illness, struggle to navigate the labyrinthine medical system. Had it not been for my sister, who has a clinical degree, I do not know how they would have fared.
Throughout, I watched good healthcare professionals who wanted to provide great care flow in and out of our lives like a crowd at rush hour; hello, I’m Susan, I’m Pilar, I’m Roger.
Here were people being asked to do the impossible—to listen, learn, and provide real care—in what little time they had. And they had so precious little. That month, I resolved to build something that’d make my mom less anxious and make her smile more. I wanted to get her more care than a care manager could actually offer, at all hours, from a kind person who always understood her present mental state (she suffers from depression) and could always knowingly pick up where they’d last left off.
I’m not unique in that desire and our family is far from alone. Half of Americans have a chronic disease and our health system’s vast resources have not translated into outcomes for all of them. At Ellipsis, we vowed to do something about it locally—at the level of care management—at the level of my own mother.
Eight years later, it is ready. We now call that resulting AI Care Manager Sage, and it’s built to connect with patients over the phone to give them round-the-clock access, to improve their outcomes. Seeing what it can do, I think it has the potential to change care.

The cost of time-poor practitioners
You don’t need to see statistics to know the story here—reach into your memory for a time you felt like the medical system wasn’t giving you the attention you needed. Or attention to someone you love.
I think it really comes down to a lack of time. If only doctors had more time, if only nurses had more time. Alas, they’re pressed from all sides and would need 27 hours per day to deliver all the guideline-recommended preventative care, according to a study of four million people. The average medical appointment demands 121 minutes from patients, between travel, paperwork, and waiting, yet the medical provider sees them for just 18 minutes of it. With all the rush, time per health concern is declining.
Patients spend 121 minutes per appointment but providers see them for just 18 minutes of it.
All the while, we know visit length is positively correlated with a patient’s satisfaction in their care—which is a major determinant in them being invested in their own recovery. To a Western medical system obsessed with saving lives, feelings seem inconsequential. But they are essential. For patients to stick with their prescribed regimen, it helps that they feel the provider is “for them.” That the people of that system care.
Further, the administrative burden upon caregivers burns them out, and when visits are shorter, doctors are more likely to prescribe inappropriately, as with two medications with contraindications.
But there has always been the tradeoff here, hasn’t there?
- If something in healthcare scales, it tends to be a poor experience.
- If it’s a good experience, it tends to be difficult to scale.
Present health system support chatbots only seem to prove the above point. No one prefers a bot that repeatedly says, “Sorry, I didn’t catch that” over help from another person. But health systems deploy them in a well-meaning attempt to scale care. Those systems based on large language models (LLMs) trained on generic datasets tend to just aggravate patients. But what can they do? The nurses they already have are overcommitted.
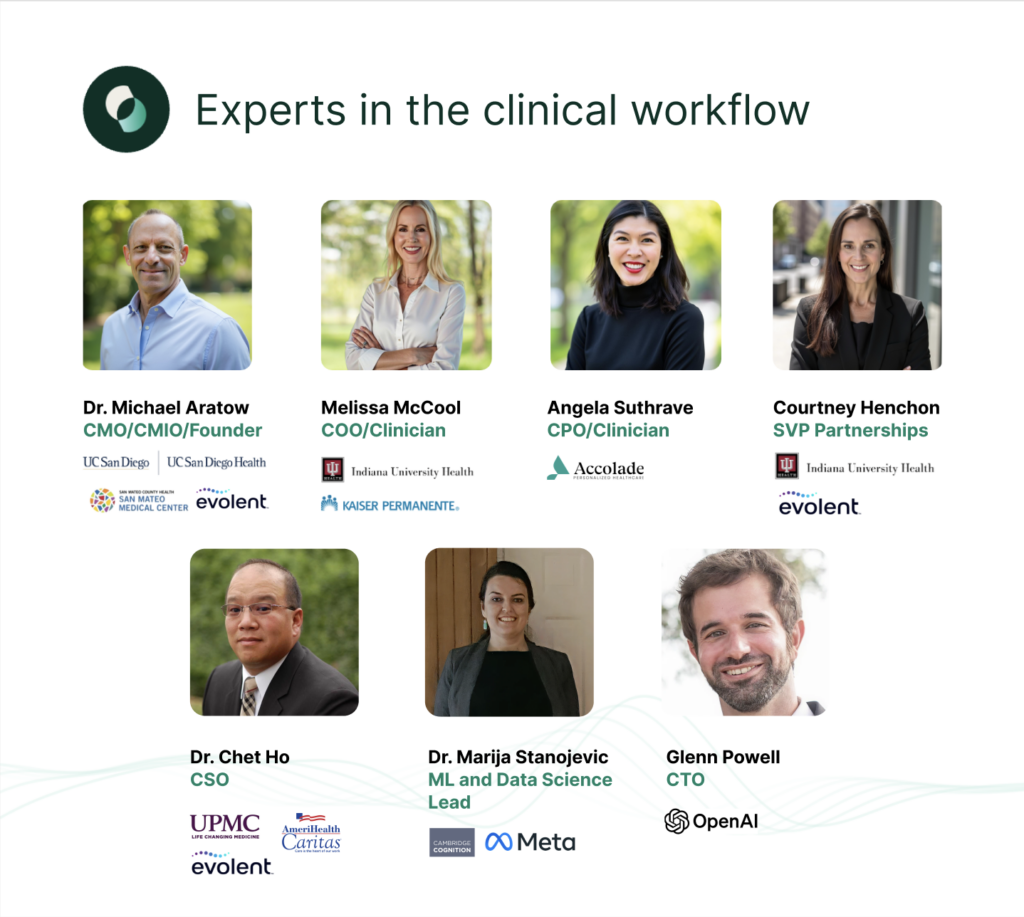
Here’s what we learned in building to help my mom: An AI agent purpose-built and trained on a dataset of millions of real patient calls can break that tradeoff if you design it to be empathetic. It is remarkable what effect a purely kind voice can have. Rather than focusing on “deflecting” calls, we focused on understanding what makes a call remarkable.
The answer is pretty simple: If the agent sounds human, though is upfront that it isn’t, and exhibits all the vocal biomarkers of “trust,” people rate the care far higher. And if it exhibits one of the most important signals of empathy, they feel listened to and cared for—namely, that it takes the infinite time with them that no caregiver ever could. It never rushes them off the phone.
If the agent sounds human and exhibits all the vocal biomarkers of “trust,” people rate the care far higher.
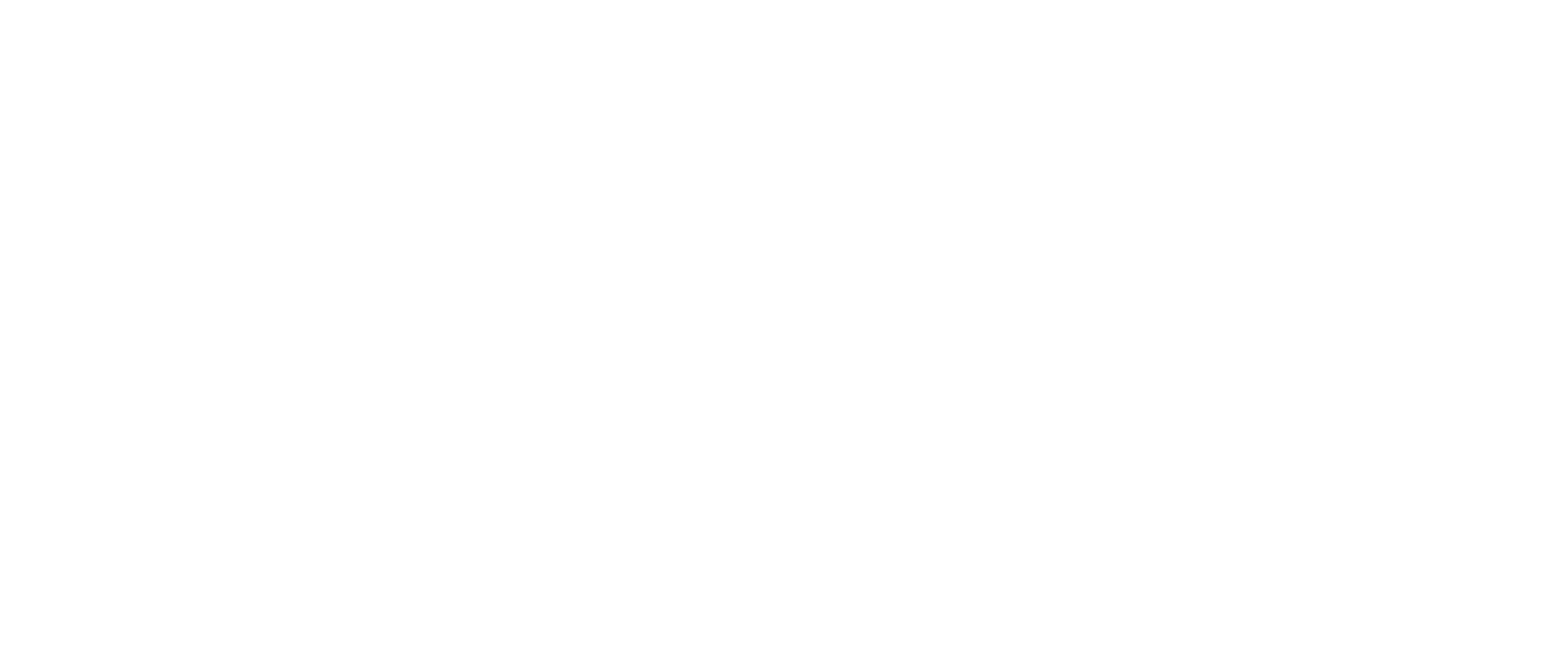
In truth, we had a bit of a head start on this—Ellipsis has been around for eight years working on a proprietary vocal biomarker technology for recognizing someone’s mental state based on their voice. And we have some rather illustrious advisors and clinical team members who were all in agreement that the patient experience would be everything.
And so it is, and I’d love you to have a listen.
Meet Sage
Have a listen to this recording, a representative sample of many, and hear how the patient responds. People often start the call saying, “I don’t have much time” and many minutes later, they are still on the phone as Sage helps them through a number of issues.
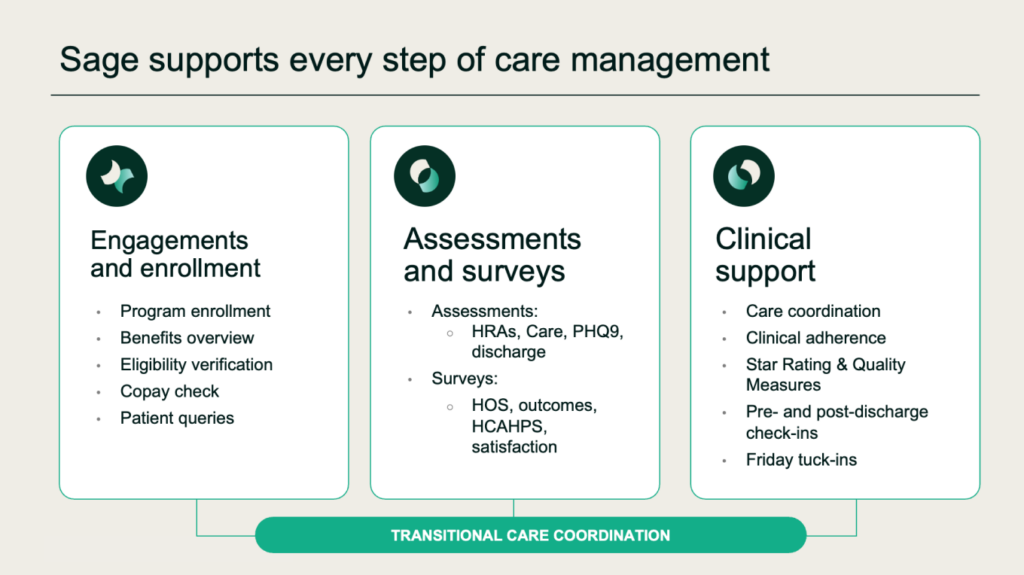
We have that initial spark of empathy. Now we can expand our mission: to improve healthcare operations and patient outcomes by giving clinical staff the phone and check-in support they need to operate at the top of their license. This technology can help health providers, plans, and care organizations raise their level of service, reduce overload, control costs, and get their ratings up.
We are often asked, “But aren’t nurses opposed to it?” So far, nurses have been emphatic about their desire for exactly this type of support.
“No nurse wants to be making 100 patient check-in calls a day, when most people don’t even pick up,” says Courtney, our SVP of partnerships, who is a registered nurse. “They’d love to have that time back and be patched through to the two calls that truly need their attention.”
So in a way, it’s empathetic to caregivers too. It fights back against the paperwork and rote tasks that keep them from practicing what they are trained to do.
Sage is built around what we’re calling an Empathy Engine:
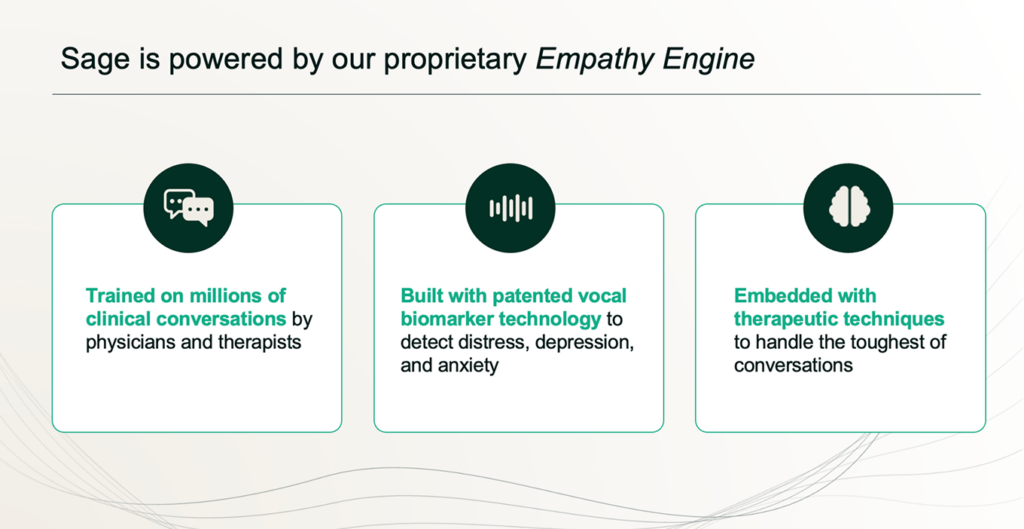
Sage doesn’t get into clinical issues—it handles the 80% of issues that don’t require a clinician. Your healthcare organization can use Sage to:
- Make care management calls following your guardrails and protocols.
- Expand your capacity and lessen your backlog to drive revenue.
- Encourage patients to engage, including for complex cases.
- Integrate with your existing workflow.
Because Sage is empathetic in a way that’s unlike any prior technology, health plans, health systems, and health providers of all sorts can finally scale care to help more patients with more use cases, so providers can focus their valuable attention.
And in the end, make more people smile, like my mom. Because they are healthier, better informed, and engaged. Which allows health providers and plans to build trust at scale and shift people’s outcomes in a positive direction, in a way that reduces cost. Schedule time with our team to listen to calls and be the judge of what effect this can have on people’s day—a care provider with an infinite capacity to listen, who’s able to build upon and react based on the patient’s medical history.
I can tell you, writing from my kitchen table right now and overhearing just one such call, that the difference is profound. I think in the next decade, we’ll be talking about the “empathy dividend” and what it can feel like when health providers and payers are able to finally empathize at scale.
If you’re a health provider, plan provider, or care management firm, and curious, Courtney, our SVP of partnerships, is a registered nurse and would be happy to chat.

Getting started is easy
Ready to see how easily and quickly you can reduce your patient backlog? Schedule a demo today.