In 2007, on a snowy road in Sweden, two buses collided head-on, killing several and injuring dozens. Seven years later, a study found that the most salient memory survivors had, aside from the pain, was the lack of compassion they felt from the overwhelmed emergency responders and hospital staff.
Imagine. Shattered glass. Shrieking metal. But it was the half-conscious feelings of momentary slights from well-meaning emergency workers that seared into their memories. The study’s authors went on to conclude that lack of compassion actually compounded those victims’ injuries and delayed their recoveries.
This is an extreme example, to be sure, but I’d argue the American medical system has drifted in that direction. A perceived lack of empathy could be causing more bodily harm than we think.
In this article, I propose a way to, in some use cases, reverse this effect without burdening practitioners. I also explore the idea that small changes in someone’s care—something as small as feeling seen and heard by a care manager—can have compounding effects that may change the entire trajectory of someone’s recovery.
The iPatient dilemma
Health plans, systems and all the workers therein are burnt out and overburdened with too many concurrent tasks. The result is they are often said to be managing “iPatient,” or the digital ghost of the person, more than they are actually hands-on and talking to them.
The average appointment takes 121 minutes of the patient’s time when you factor in travel, paperwork, payment, and waiting. But the provider sees them for just a slim 18 minutes of that total. The time spent per concern is falling and shorter visit lengths are associated with a higher likelihood that doctors inappropriately prescribe medications.
This makes logical sense: Less time per patient per concern means more patient risk. It also means terser interactions.
Merely spending time is one of the top factors in determining whether a patient is cared for, but also feels cared for. Whereas unsympathetic interactions—which does not mean the practitioner doesn’t care, only that they aren’t displaying the signals of such—turn patients off of the system and make them less likely to follow their care regimens.
Less time per patient per concern means more patient risk. It also means terser interactions.
A patient who feels their doctor doesn’t like them is less likely to believe their diagnosis, take their medications, and make the next appointment. Just as consumers vote with their feet, so too do patients—they’re apt to ask to switch medical providers, further fragmenting their care.
Multiply that over a system of such complexity and cost and you get declining outcomes. And the question is, what would it take to reverse it?
Health providers can earn an empathy dividend
Human sensory perception is at once highly advanced and highly flawed. Most of us can recognize the most subtle changes in someone else’s demeanor, yet we’re often very wrong about what’s happening inside their head—we tend to think other people dislike us more than is true and fabricate stories to look for reinforcing evidence.
This matters in care. In a study, patients who rated their doctor as unlikable were more likely to look outside the medical system for answers, try non-proven therapies, and believe in the positive effects of those therapies. Once doubt has taken hold, they view all following recommendations with incredulity. Multiply this across the entire system, compounding with each interaction—where each neutral or negative interaction worsens care from there on.
But could we get the effects of this working in the opposite direction? Patient “paranoia” has a lesser-known antonym—patient “pronia,” or the belief that the world is conspiring to help you.
What would a world of patient pronia look like? What if healthcare workers could spend more time, rather than always rushing to the next task? What if caregivers had fuller context and could better pick up exactly where they and the patient last left off? What if they could signal that they care as much as they actually do?
I believe if you could create this sort of system, the desperate search for non-proven therapies would collapse into the opposite: those patients referring others to their doctor. The compounding effects from mere positive feelings could be enormous, just in the sense that patients who feel liked participate more in their own care and lift a great weight off the medical system.
That’s what we are trying to build, at least partly. I started Ellipsis while observing my mom, who suffers from two chronic conditions, try to navigate the care system. I asked, what if we started as local as possible and tried to create an AI voice agent that could make my mom smile more because she feels the care she receives is empathetic, generous, and of high quality?
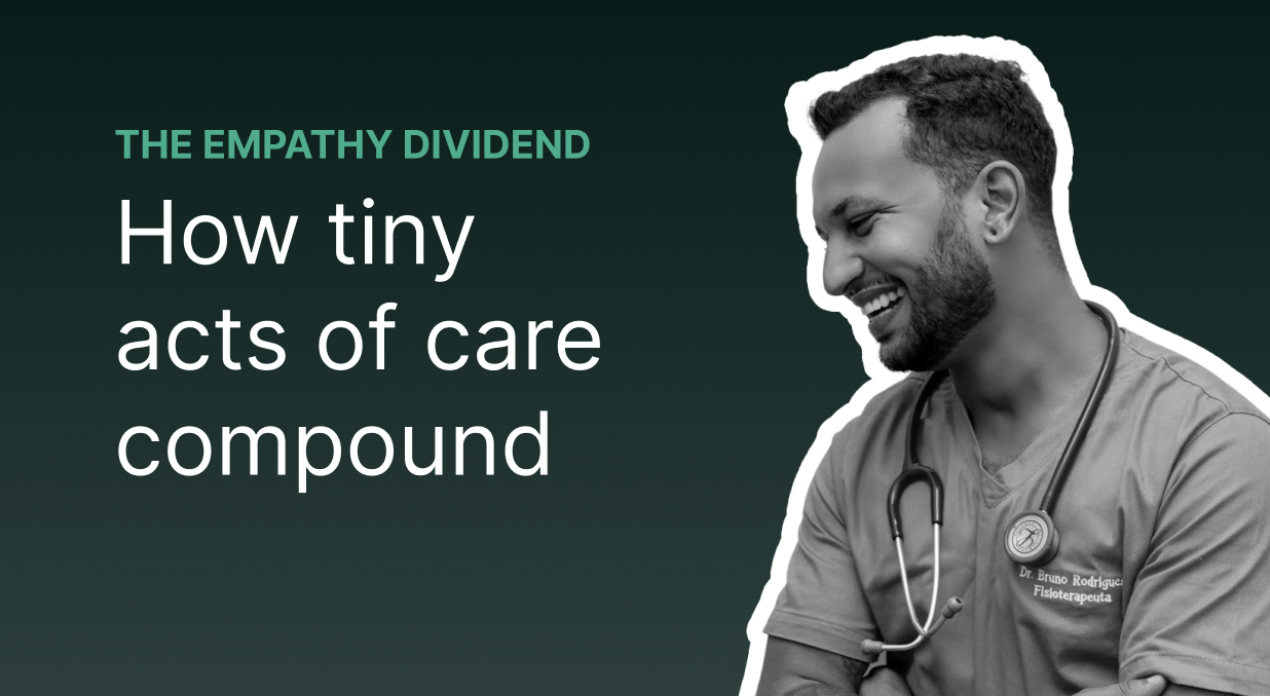
We’ve built an AI care manager that seems to have done what none other has done before—patients feel it empathizes with them. It exhibits all the vocal biomarkers of “trust” and though people may ask, “Are you a computer?” its tonally appropriate reply, “Yes, and I am here to help” is enough that they carry through with the call and feel great thereafter.

Sage is built upon an empathy engine that we’ve trained on millions of actual clinical calls, with embedded therapeutic techniques to handle the toughest conversations. Sage doesn’t get into sensitive clinical issues—it follows your protocols and handles the 80% of calls that do not require a licensed practitioner. That relieves a great deal of stress from clinicians. So while Sage is delivering positive feelings to patients, it’s allowing practitioners to rest as well.
The effect we are seeing on actual practitioners is profound. Relieved of making 100 check-in calls with patients, most of whom won’t respond, a nurse practitioner can spread their time more evenly across patients. (And actually take lunch.) A health insurance provider can reach at-risk patients and programmatically schedule follow-ups at scale to ensure people remain engaged. Doctors can come to patient visits better informed thanks to the brief, auto-generated summary of an hour-long conversation the patient had with Sage. And though the doctor still only has 18 minutes to give, those 18 minutes are more effective—and feel better.
This is the Sage effect we expect to see: Health providers are noticing that patients are coming back to them with a lightness. An eagerness. An engagedness. Because that infinitely scalable empathetic care manager conveyed the heart of what this system has been trying to do for them all along, but wasn’t signaling: Care.
Imagine those positive feelings, that your health plan or system is “for them,” multiplied and compounded over years and lives.
I call that the empathy dividend. It’s an investment in delivering and overtly conveying the sense of care that’s true to your organization, across every touchpoint, and giving people that feeling of being seen and heard.
If this idea interests you as much as it interests me, and you are an investor, provider, or builder in this space, we’d love to hear from you. Please get in touch.
Latest insights
How does Ellipsis Health keep sensitive data safe? 9 questions answered
From our beginnings in 2017, we have put privacy, consent, and data security at the forefront of our work.

What are upcoming advances for speech-based depression and anxiety screening?
At Ellipsis Health, we’ve been looking back at some of the breakthrough applications of vocal biomarker technology that we’ve unlocked alongside our health plan, health system, academic medical center, and digital health partners.

Getting started is easy.
Ready to see how easily and quickly you can reduce your patient backlog? Schedule a demo today.